Description
Chondromyxoid fibroma, or CMF, is a very rare, non-cancerous bone tumor that usually affects teenagers and young adults in their 20s. It is seen more often in males. These tumors are most commonly found in the long bones of the legs, like the femur (thigh bone) and tibia (shin bone), and can cause the bone to look expanded or have a bubbly appearance on imaging. Although it's less common, CMF can also occur in older patients (in their 50s or 60s), and in those cases it can frequently appear in the pelvic bones.
Symptoms
Chondromyxoid fibromas (CMF) can sometimes grow quite large and may cause dull, achy pain in the area. Depending on the size and location of the tumor, some patients may notice that one leg looks slightly bigger or feels stiffer than the other. Because these tumors often grow in the bones of the legs, walking or running can become uncomfortable or painful. It’s rare to see redness or other skin changes with these tumors. Since CMF can make the bone weaker there’s a chance the bone could break (this is called a pathologic fracture). Ideally, the tumor is found and treated before this happens, because removing it before a break usually means less pain and faster recovery.
Examination
In young adults with CMF of the lower extremity, there may be swelling and limited range of motion in the area. In older adults with CMF of the pelvis, these patients may not experience any symptoms, unless the tumor has grown large enough to compress nearby abdominal structures (i.e., urinary retention, bowel obstruction, etc.)
Tests
The first step in diagnosing chondromyxoid fibroma (CMF) is usually an X-ray of the affected area. In young adults, CMF can look very similar on X-rays to other non-cancerous bone tumors that are common in this age group, such as non-ossifying fibromas or aneurysmal bone cysts. However, these tumors look different when examined under a microscope. Additional imaging—like a CT scan or an MRI with contrast dye—is often needed to get a clearer picture of the tumor.
In older adults, especially when CMF occurs in the pelvis, the tumor can look very much like a more serious bone cancer called chondrosarcoma. Because of this, a biopsy (a procedure where a small sample of the tumor is taken and examined under a microscope) is usually needed to confirm the diagnosis before making any treatment decisions.
Images
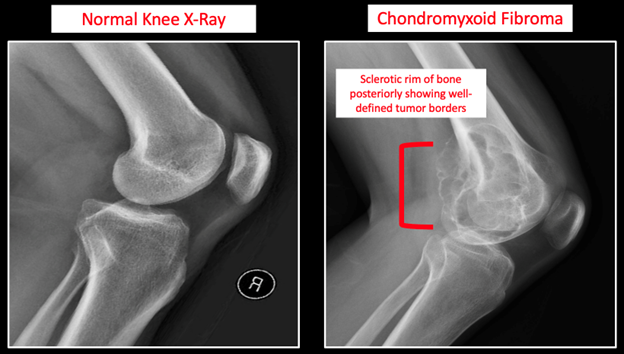
On X-rays, CMFs usually appear as well-defined, bubbly or lobulated areas within the bone. These tumors often cause the bone to expand slightly and may have a thin rim of bone around them. On MRI scans, the tumor may show a mix of different textures, reflecting the combination of cartilage, fibrous tissue, and fluid-like material inside the tumor. MRI is especially helpful in showing how the tumor interacts with nearby soft tissues and joints. A CT scan can provide additional detail about the bone itself, especially in more complex areas like the pelvis.
Figure 1. Anterior-posterior (AP) imaging comparing a normal knee X-ray to a knee with a chondromyxoid fibroma
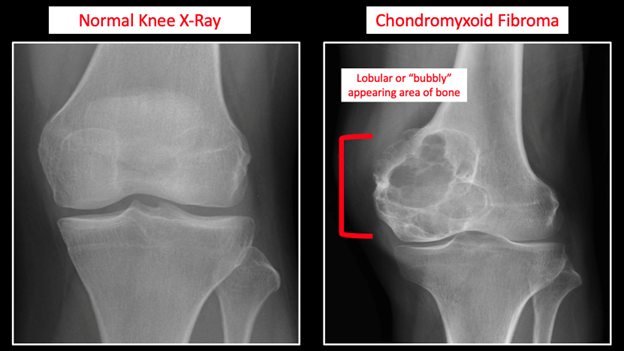
Figure 2. Anterior-posterior (AP) imaging comparing a normal knee X-ray to a knee with a chondromyxoid fibroma.
Prognosis
Chondromyxoid fibromas (CMFs) have good prognosis. They are benign tumors (they are not cancer) and therefore do not spread to other areas of the body. The main treatment for CMF is surgery. In most cases, the surgeon removes the tumor by scraping it out of the bone in a procedure called curettage. To lower the chance of the tumor coming back, the area is sometimes treated with special tools or medicines during surgery, and may be filled with bone graft or bone cement afterward. In rare cases—especially if the tumor is very large, has come back, or is in a difficult spot—the surgeon may need to remove a larger section of bone. After surgery, most people recover well and can return to normal activities. Regular follow-up visits with imaging are important to make sure the tumor doesn’t return. For this reason, it is highly recommended that you be treated by an orthopedic oncologist who specializes in treating bone tumors.
More Information:
- https://orthoinfo.aaos.org/en/diseases--conditions/chondromyxoid-fibroma
- https://www.cancer.gov/pediatric-adult-rare-tumor/rare-tumors/rare-bone-tumors/chondromyxoid-fibroma
This is not intended as a substitute for professional medical advice and does not provide advice on treatments or conditions for individual patients. All health and treatment decisions must be made in consultation with your physician(s), utilizing your specific medical information. Inclusion in this is not a recommendation of any product, treatment, physician or hospital.


